Más Información

VIDEO: Avión militar con miles de pesos en efectivo se accidenta en Bolivia; policía dispersa con gas lacrimógeno rapiña

Artículo 19 exige investigación y protección al comunicador Víctor Badillo; fue atacado en instalaciones de su medio en Nuevo León
Hallan cuerpos de dos mujeres en caminos de terracería en Silao e Irapuato; difunden fichas de búsqueda de otras 12 jóvenes
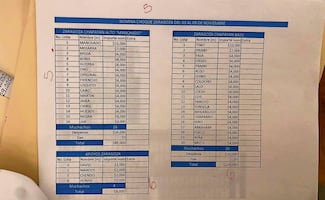
Harfuch: se investiga narconómina de "El Mencho" dada a conocer por EL UNIVERSAL; no hay funcionarios ligados a indagatorias, indica
Silent hypoxia
began having an echo in the context of the pandemic. Medical experts around the world began to notice that some patients with COVID-19 had a low level of oxygen saturation in the blood but without showing other common symptoms, such as the lack of air, which made them arrive later to the emergency room.
Experts began to dwell into the origin of this condition and the usefulness of pulse oximeters began being spread. Pulse oximeters are the instrument used to measure the levels of oxygen in the blood and are not part of the glossary linked to the development of the new virus.
Dr. Sergio Alberto Mendoza Álvarez, a professor of the Postgraduate Studies Division of the School of Medicine, mentions that before the arrival of SARS-CoV-2, the concept of silent hypoxia rare Heard of because the clinical pictures linked to pneumonia very mainly histological, that is, changes at the lung tissue, but the mechanisms of pneumonia in COVID-19 are also determined by other factors, both immune and related to blood flow.
For Mendoza Álvarez, hypoxia in patients with COVID-19 has three mechanisms, one of them are the microthrombi in the lung capillaries. “It has been detected that there are thrombi that block the arterial circulation. Blood flow to the alveoli is lessened and it causes low oxygenation.” The physician mentions that the immune disorder also causes the body’s defense to attack the lung tissue in a pro-inflammatory cascade that generates chaos with a rise of inflammatory cells. The third cause for the reduction of oxygen available for the body’s cells are atypical bacterias that add to the viral infection and that can also jeopardize oxygenation to the alveoli.
Recommended:
Recently, the medical director of the American Lung Association, Albert Rizzo, issued a statement in which he talks, among other things, about the possible causes of hypoxia being “silent.” He said that the lungs initially keep “answering” for they are not still rigid nor full of liquid. This means that patients can still expel carbon dioxide and thus, they do not feel short of breath.
For his part, Mendoza Álvarez mentions that when patients with COVID-19 have an oxygen saturation below the minimum levels, they do not often have the usual symptoms, such as lack of air and mental confusion, which can delay a timely treatment. “They only mention a small pressure on their chest, but sometimes it’s not even that.” Nevertheless, patients begin coughing, which becomes severe in the following days. When they arrive at an emergency room, oxygenation has gone below the minimum levels.
Measuring
People were not previously acquainted with pulse oximeters , but the pandemic made them almost as popular as thermometers. Pulse oxymeters work as a kind of clamp that is put on a finger and uses light emission to capture the hemoglobin absorption range that is translated into a numerical range. It is considered that oxygen saturation is located between 98% and 94% for healthy adults with 88Ç% as a minimum range, but there are variations that must be interpreted by experts.
The medical director of the American Lung Association stresses that measuring the levels of oxygen in the blood must not be a way for patients to self-detect COVID-19 .
The association believes it is best to contact an expert in case there is any suspicion of the disease instead of only relying on pulse oximeters. “ Silent hypoxia is not usually an early sign in patients with COVID-19 . They often arrive in the emergency room for other reasons, such as fever, muscle pain, or fatigue. For the most part, when a patient begins showing silent hypoxia, they already have other symptoms related to the virus”
Recommended:
Mendoza Álvarez agrees with the latter since pulse oximeters have become very useful for doctors in the objective evaluation of e¡oxygenation but in the framework of other observations. “Fever and couching are directly associated with low oxygenation; it is unlikely for a patient without these symptoms to show a range below 88%.”
He explains that when a patient has a fever, the shivers themselves will lower the oxygenation because there is no proper transport of oxygen due to the change of temperature in the body. If the temperature is controlled, oxygenation can return to a normal parameter. In the case of dry coughing that increases, the lack of oxygenation and progress in the clinical picture are more evident.”
The professor insists on properly monitoring dry coughing during the first week along with the rest of the symptoms with a specialist since the second or third day of showing suspicious symptoms for there is more chance of complication between days seven and 12. It is likely that the doctor will suggest complementary tests in case coughing increases and there is a lack of air.
The tests include a chest CT-scan and an arterial blood gas to identify the lung damage and to know the apparently silent pneumonia. This will help to make decisions regarding the proper medication so that the patient does not present further complications that would require intubation.
Recommended:
“It must always be checked with doctors to evaluate the general picture because, without the proper interpretation, the instrument does not work,” says the expert and adds that, in this way, the medical instrument can become a truly useful ally during different stages of the disease. It must not be used for self-diagnosis, but he mentions that it has pre, intra, and post-hospital use because it does not only help to monitor the disease but it also monitors the results of lung rehabilitation and the functional recovery of the patient to determine their oxygen requirement until it is no longer needed.
mp
Noticias según tus intereses
[Publicidad]
[Publicidad]